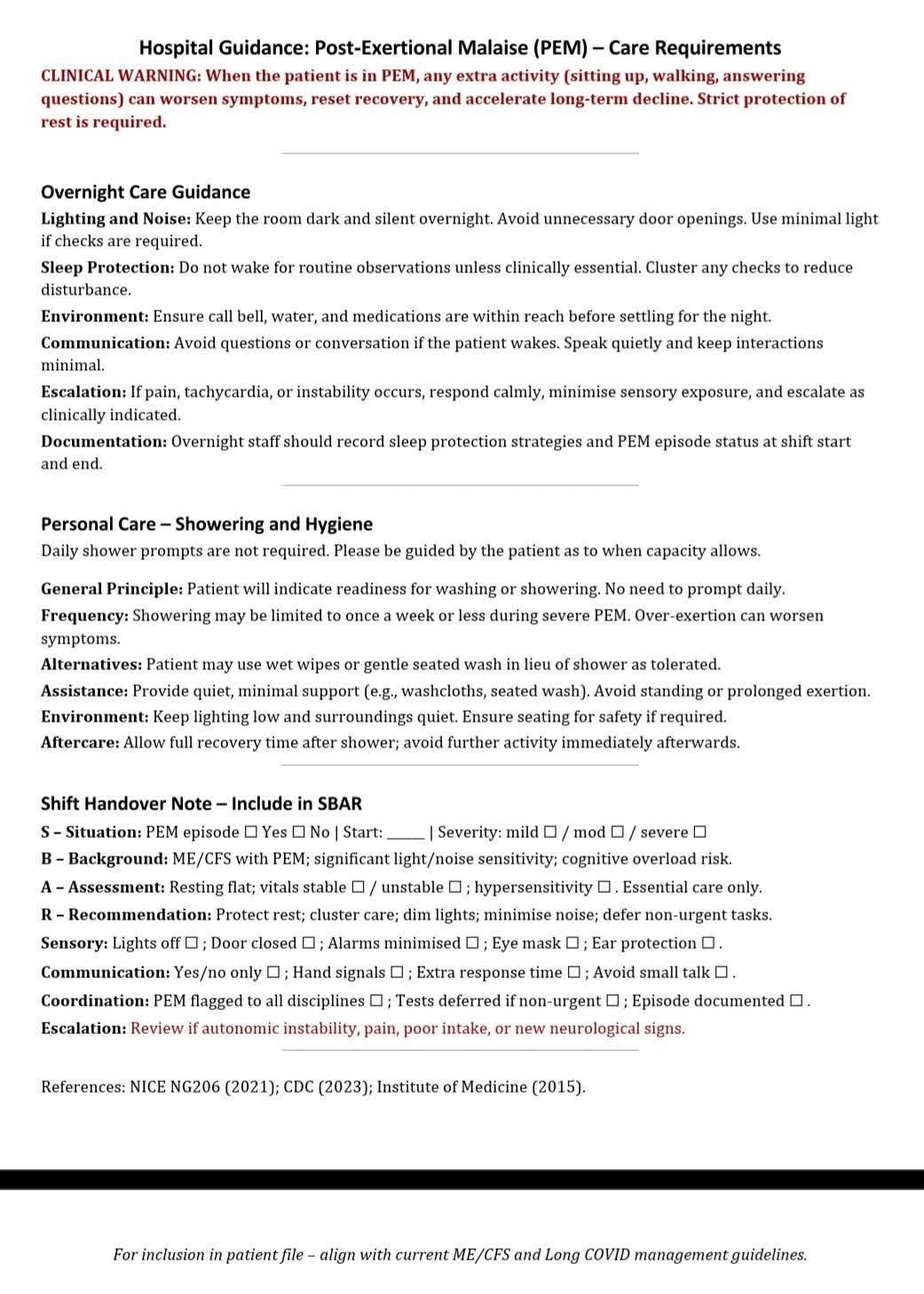
Hospital Guidance: Post-Exertional Malaise (PEM) - Care Requirements
CLINICAL WARNING: When the patient is in PEM, any extra activity (sitting up, walking, answering questions) can worsen symptoms, reset recovery, and accelerate long-term decline. Strict protection of rest is required.
Overnight Care Guidance
Lighting and Noise: Keep the room dark and silent overnight. Avoid unnecessary door openings. Use minimal light if checks are required.
Sleep Protection: Do not wake for routine observations unless clinically essential. Cluster any checks to reduce disturbance.
Environment: Ensure call bell, water, and medications are within reach before settling for the night.
Communication: Avoid questions or conversation if the patient wakes. Speak quietly and keep interactions minimal.
Escalation: If pain, tachycardia, or instability occurs, respond calmly, minimise sensory exposure, and escalate as clinically indicated.
Documentation: Overnight staff should record sleep protection strategies and PEM episode status at shift start and end.
Personal Care - Showering and Hygiene
Daily shower prompts are not required. Please be guided by the patient as to when capacity allows.
General Principle: Patient will indicate readiness for washing or showering. No need to prompt daily. Frequency: Showering may be limited to once a week or less during severe PEM. Over-exertion can worsen symptoms.
Alternatives: Patient may use wet wipes or gentle seated wash in lieu of shower as tolerated.