Affinity groups
from How To Talk To Your Loved Ones About Covid (covid.tips)
https://covid.tips/#affinity-groups
If there are vulnerable and oppressed groups that the person you’re talking with has an affinity with, invite them to see how wearing a mask is a crucial step toward supporting that community, and share how Covid is affecting that group in particular (see our Affinity group resources section). If the people you’re talking to are part of an oppressed group themselves, it’s likely that they already understand many of the ways in which the government has let their communities down before. Remember: our struggles are all linked, and the point of considering affinity groups is not for sympathy or charity but for solidarity and connectedness.
If you have come here to help me, you are wasting your time. But if you have come because your liberation is bound up with mine, then let us work together.
-Aboriginal activist group, QLD Australia (1970s)
There is no such thing as a single-issue struggle because we do not live single-issue lives.
-Audre Lorde
We need to move away from framing our decision to mask as doing so mainly out of charity for "the most vulnerable." Framing Covid as something that only affects the sick has led to where we are right now. The policy decisions that work to normalize Covid and downplay its risk to the working class benefit from the pre-existing political and economic conditions that have long been used to control working people. These are intentionally designed policies that serve to utilize the disabled population as a threat to control and disempower the working class.
“Public policy that equates disablement with poverty means that becoming disabled (a nonworker) translates into a life of financial hardship, whether one has public assistance or not, and generates a very realistic fear in workers for becoming disabled”
“If workers were provided with a federal social safety net that adequately protected them through unemployment, sickness, disability, and old age, then business would have less control over the workforce because labor would gain a stronger position…Business retains its power over the working class through a fear of destitution that would be weakened if the safety net were to actually become safe.”
-Marta Russell, “Marxism and Disability,” as referenced in this article
So of course, in a society that equates medical aids with disability and illness, it is easy to consider mask wearing and other Covid precautions as something that is only for the “vulnerable” or disabled, a category that is understandably feared by the working class due to the political and economic realities of being disabled under a system that uses your suffering for leverage and profit.
We are all at risk from Covid. And we all deserve freedom from that risk.
The framing of risk as exclusive to vulnerable people leverages pre-existing political and economic pressures around disability to allow people to continue to see themselves as separate from those considered “at-risk”, “vulnerable” or disabled and gain a false feeling of safety. It has never been true that only the “sick and elderly” are at risk—and it wouldn’t be okay to abandon them if they were—but many people still believe this lie in order to feel safe.
Feeling safe and being safe are not the same thing.
Safety comes from taking actions that protect the whole community. Covid continues to wreak havoc on the global population—and the death toll is much higher than original estimates suggested. According to The Economist in November of 2022:
Although the official number of deaths caused by covid-19 is now 7m, our single best estimate is that the actual toll is 27.4m people. We find that there is a 95% chance that the true value lies between 18.2m and 33.5m additional deaths.
Source: The Economist
The death toll continues to climb. Many millions more have Long Covid as a result of these governmental failures. The policy choices that have been put in place have never been about protecting our safety, and they have never been about protecting our collective interests. Once again, it has been about profit over people.
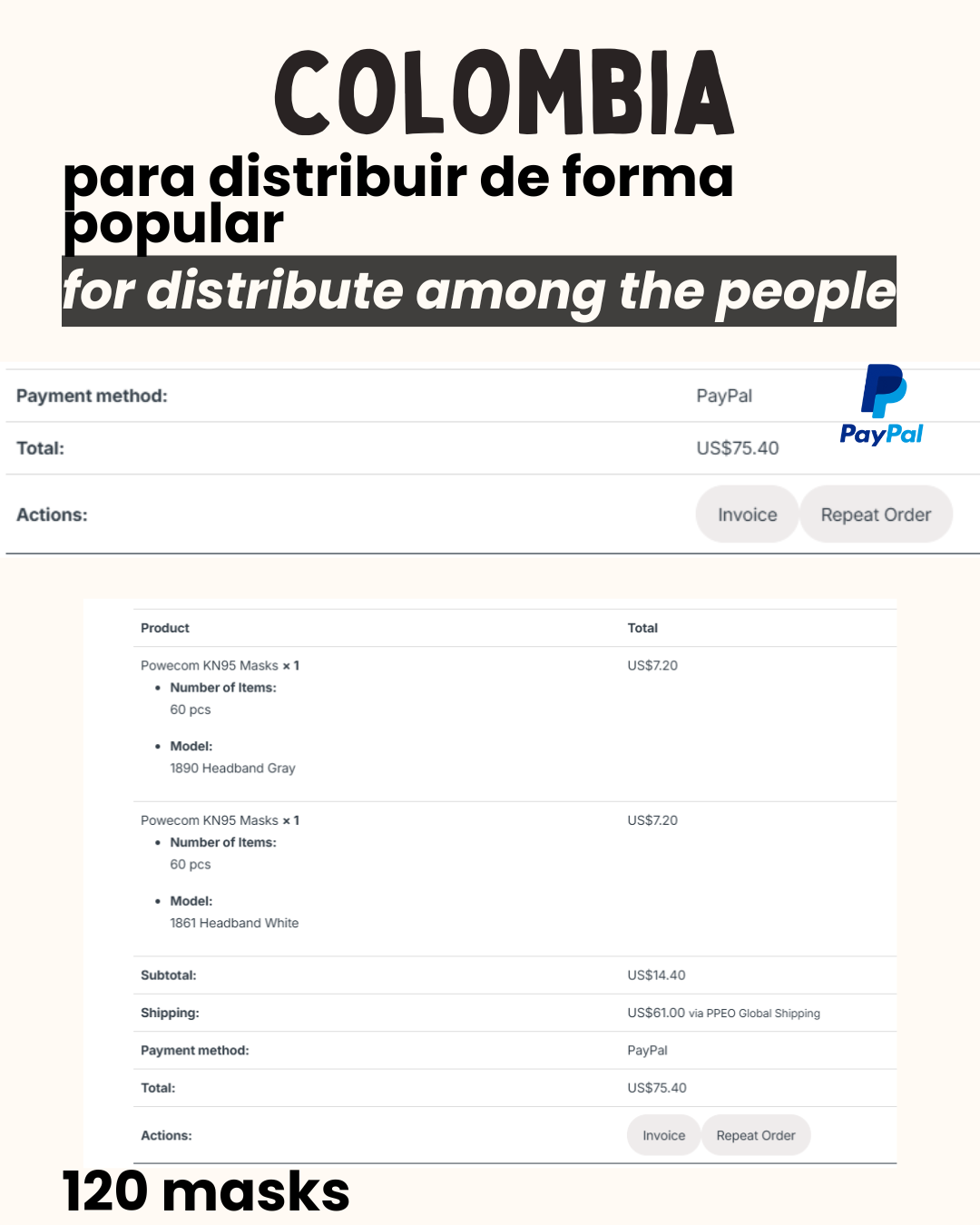
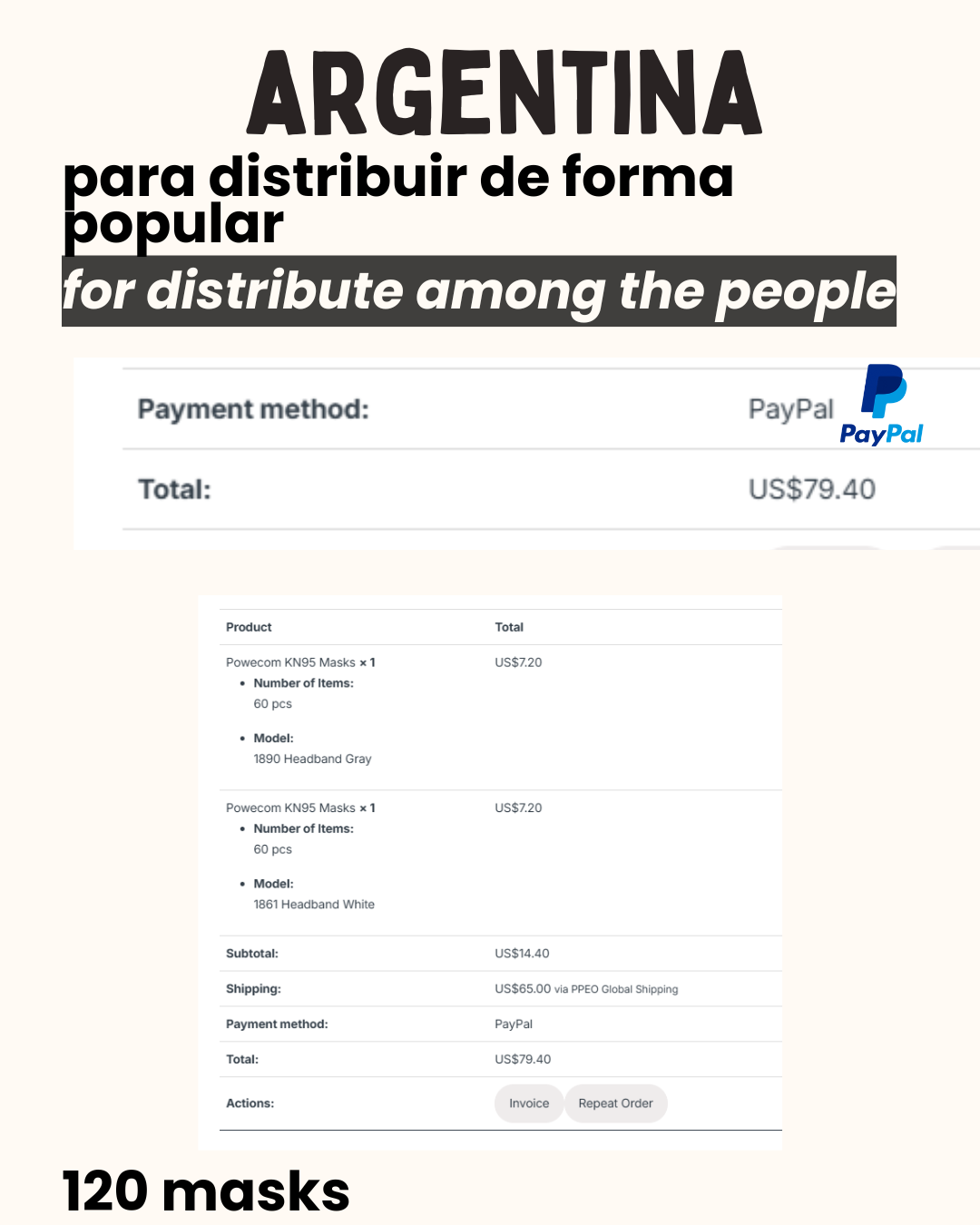
Masks are community care❤️🔥😷 free masks: maskbloc.org
• Remember: covid is not over, 50% of infections are asymptomatic, minimum 10% of infections end up in long COVID, re-infections wreck us, COVID spreads and moves like cigarette smoke, think of the people around you and you as people who are all day smoking, it becomes more visual to understand how COVID moves.
• There is no way to “train” the immune system because it is not a muscle. there is a common misconception that exposure to harmful germs strengthens the immune system. viral diseases like COVID, flu, measles weaken the immune system, leaving the possibility of lasting damage. The reality is that you don't build your immunity with repeated infections, vaccines strengthen the immune system by teaching it to recognize pathogens without all the risks. Focusing on infection prevention is key.
• Rapid antigen tests give many false negatives.
• Solving the pandemic was never in the cards for the capitalist world.
• Instead, the explicit goal of the ruling class has been to make the pandemic simply disappear from public perception. Any reminder of the existence of a highly-transmissible, highly-dangerous, mass-disabling disease could trigger panic, or worse: organized, militant labor action. Averting this crisis required a careful campaign of culture-crafting; the people themselves needed to become convinced that there was no reason to fight. Consent for protracted mass infection needed to be manufactured.
“The cold truth of the matter is that the motive behind COVID minimization is greed and social control. (…) Solving the pandemic was never in the cards for the capitalist world. Instead, the explicit goal of the ruling class has been to make the pandemic simply disappear from public perception.” Let Them Eat Plague! http://clarion.unity-struggle-unity.org/
#MaskUp #WearAMask #CovidRealist #CovidIsAirbone #LongCovid #YallMasking #DisabledLiberation #DisabilityJustice
.